When attempts with medications and lasers fail to adequately control one’s eye pressure or glaucoma, your doctor may recommend glaucoma surgery. This includes incisional glaucoma surgery and high-powered lasers, both performed in an ambulatory surgery center. There are multiple different types of glaucoma surgery. It does not reverse glaucomatous damage that has already occurred.
The goal of surgery is to halt the disease process by lowering the intraocular pressure, thus preventing optic nerve damage and worsening vision loss.
Types of Glaucoma Surgery
The goal of surgery is to lower intraocular pressure. This can be done a few different ways:

- Improve the drainage of aqueous using its natural or physiological pathway. This involves working with the trabecular meshwork and schlemm’s canal (drainage system of the eye). Examples include goniotomy, Omni® canaloplasty/trabeculotomy, GATT, istent®, and Hydrus®.
- Creating an alternative drainage channel bypassing the traditional pathway and allowing aqueous to leave the eye resulting in lower pressure (Trabeculectomy, Glaucoma drainage implant/tube, and Xen® gel stent).
- Decreasing the amount of aqueous being pumped into the eye thus resulting in lower intraocular pressure (Transscleral and endoscopic cyclophotocoagulation).
Glaucoma surgery can be further broken down into:
Micro-invasive glaucoma surgery (MIGS)
- Goniotomy (TrabEx® and Kahook Dual Blade®)
- Hydrus® microstent
- Istent®
- GATT (Goniotomy Assisted Transluminal Trabeculotomy)
- Omni® (Canaloplasty/trabeculotomy)
- ECP (Endoscopic cyclophotocoagulation)
- CPC (Transscleral cyclophotocoagulation)
- Xen® Gel Stent
Traditional glaucoma surgery
Goniotomy (TrabEx® and Kahook Dual Blade Glide®)
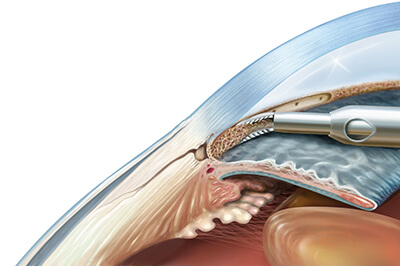
Goniotomy is a well established surgical technique done using a single-use surgical device, such as the Kahook Dual Blade Glide® (KDB) and the TrabEx®. They both feature a dual-blade design, done as a stand alone procedure or in conjunction with cataract surgery. When done with cataract surgery, it is commonly done after the cataract is removed by using the same clear corneal incision. Using a mirrored gonio lens for visualization, these devices are inserted into the anterior chamber of the eye and the trabecular meshwork is excised allowing better axis for the aqueous to schlemm’s canal and the collector channels. If successful, this results in better outflow and lower intraocular pressure. This procedure is minimally invasive and does not involve opening up the conjunctival tissue, making future glaucoma surgeries simpler if necessary.
Both TrabEx® and Kahook Dual Blade Glide® goniotomy are done in an ambulatory surgery center under local anesthesia and light intravenous sedation (like cataract surgery). In some cases an eye block may be done for additional anesthesia. Following this procedure you will be using post operative medications in addition to your glaucoma drops. If successful, you might be able to eliminate some of your glaucoma eye drops. Your surgeon will examine you the following day.
Hydrus® microstent
The Hydrus® microstent is an FDA-approved device implanted at the time of cataract surgery through the trabecular meshwork into schlemm’s canal to decrease intraocular pressure. The 8mm device is made of nitinol and works via bypassing the trabecular meshwork and dilating schlemm’s canal allowing better aqueous outflow and ultimately lower eye pressure. The device is implanted using the same incision used for the cataract extraction. This procedure is minimally invasive and does not involve opening up the conjunctival tissue, making future glaucoma surgeries simpler if necessary. Patients can safely undergo MRI in most circumstances. If there are any questions regarding this please contact our office or visit the Hydrus® information page https://www.ivantisinc.com/isi/.
The Hydrus® Microstent is done in an ambulatory surgery center under local anesthesia and light intravenous sedation (like cataract surgery). In some cases an eye block may be done for additional anesthesia. Following this procedure you will be using post operative medications in addition to your glaucoma drops. If successful, you might be able to eliminate some of your glaucoma eye drops. Your surgeon will examine you the following day.
Istent®
The iStent inject® W is an FDA-approved device implanted at the time of cataract surgery, using the same cataract incision. The newest device includes two titanium stents, less than 1mm, that are implanted through the trabecular meshwork into schlemm’s canal 2 to 3 clock hours apart to enhance aqueous outflow and lower intraocular pressure. This procedure is minimally invasive and does not involve opening up the conjunctival tissue, making future glaucoma surgeries simpler if necessary. Patients can safely undergo MRI in most circumstances. If there are any questions regarding this please contact our office or visit the Istent® information page https://www.glaukos.com/dfu-mri-information.
The istent inject® W is done in an ambulatory surgery center under local anesthesia and light intravenous sedation (like cataract surgery). In some cases an eye block may be done for additional anesthesia. Following this procedure you will be using post operative medications in addition to your glaucoma drops. If successful, you might be able to eliminate some of your glaucoma eye drops. Your surgeon will examine you the following day.
GATT (Goniotomy Assisted Transluminal Trabeculotomy)
GATT is a minimally invasive glaucoma surgery performed using small micro-incisions in the cornea. After entering the eye, the trabecular meshwork is pierced, schlemm’s canal is then cannulated 360 degrees, and ultimately unroofed. This allows the whole drainage system of the eye to be targeted, allowing increased aqueous outflow and reduction of intraocular pressure. This procedure is minimally invasive and does not involve opening up the conjunctival tissue, making future glaucoma surgeries simpler if necessary.
GATT is done in an ambulatory surgery center under local anesthesia and light intravenous sedation (like cataract surgery). In some cases an eye block may be done for additional anesthesia. Following this procedure you will be using post operative medications in addition to your glaucoma drops. If successful, you might be able to eliminate some of your glaucoma eye drops. Your surgeon will examine you the following day.
Omni® (Canaloplasty/trabeculotomy)
The Omni® surgical system is a minimally invasive implant free procedure using a small microcatheter through a small corneal incision. It can be done as a stand alone procedure or in conjunction with cataract surgery. The device penetrates the trabecular meshwork, catheterizes Schlemm’s canal, dilates the canal and distal collector channels using viscoelastic (canaloplasty), and ultimately unroofs the trabecular meshwork (trabeculotomy). This results in lowering resistance of aqueous outflow at multiple sites of the drainage system, leading to lower intraocular pressure. This procedure is minimally invasive and does not involve opening up the conjunctival tissue, making future glaucoma surgeries simpler if necessary.
Omni® is done in an ambulatory surgery center under local anesthesia and light intravenous sedation (like cataract surgery). In some cases an eye block may be done for additional anesthesia. Following this procedure you will be using post operative medications in addition to your glaucoma drops. If successful, you might be able to eliminate some of your glaucoma eye drops. Your surgeon will examine you the following day.
ECP (Endoscopic cyclophotocoagulation)
ECP is most often done in conjunction with cataract surgery using the same incision. Following removal of the cataract a small probe with a camera is inserted into the eye. The probe is connected to a laser with fiber-optic cables that allows laser energy to be delivered to the ciliary body, which is the structure producing fluid and pressurizing the eye. As a result it causes coagulation of the ciliary body and a reduction of intraocular fluid, leading to reduced eye pressure. The laser energy can be titrated to achieve light blanching of the ciliary processes, which is directly visualized on a monitor during the procedure. This portion of the surgery takes only a few minutes and should cause minimal if any pain. This procedure is minimally invasive and does not involve opening up the conjunctival tissue, making future glaucoma surgeries simpler if necessary.
ECP is done in an ambulatory surgery center under local anesthesia and light intravenous sedation (like routine cataract surgery). In some cases an eye block may be done for additional anesthesia. Following this procedure you will be using post operative medications in addition to your glaucoma drops. It may take 6-8 weeks before the final outcome of the procedure is known. If successful, you might be able to eliminate some of your glaucoma eye drops. Your surgeon will examine you the following day.
CPC (Transscleral cyclophotocoagulation)
Transscleral cyclophotocoagulation (CPC) is often done as a stand alone procedure to lower intraocular pressure. Like ECP it works by shutting down the cells in the eye that produce the intraocular fluid (ciliary body). It is generally used in cases of advanced glaucoma or eyes that have had previous glaucoma surgeries. It is done in an ambulatory surgery center generally under IV sedation and an eye block. Following anesthesia, the surgeon will place the probe on the surface of the eye near the limbus (cornea/sclera junction), and then apply the laser energy. Generally the surgeon will treat approximately 20 to 30 laser spots, 360 degrees, avoiding sites of previous surgeries and sensory nerves. The laser energy is transmitted through the tissue and into the ciliary body, resulting in coagulation and decreased production of intraocular fluid to lower the eye pressure.
No incisions or cuts into the eye are necessary and the surgeon can easily titrate the laser energy and treatment intensity based upon the patient’s needs. This procedure can be repeated and the response may not be determined for a few weeks post operatively. You will leave the surgery center with an eye patch and generally will start drops later that day or the following day. Your surgeon will examine you the following day to check your pressure.
Xen® Gel Stent
The Xen® Gel Stent is a micro surgical implant used to lower eye pressure in the setting of more moderate or advanced glaucomas. The stent bypasses the traditional outflow pathway, allowing fluid to get out of the eye, where it drains into the subconjunctival space (filtering bleb) and eventually is absorbed back into the body. It can be done as a stand alone procedure or in conjunction with cataract surgery. The Xen® injector can implant the stent via a small corneal incision (internal approach) or externally through the sclera and into the anterior chamber. When done externally, the conjunctival tissue does need to be opened up similar to traditional glaucoma filtering surgeries. Similar to the traditional glaucoma filtering surgery trabeculectomy, the surgeon will use the anti-scarring medication mitomycin-C (MMC) or 5-Fluorouracil (5-FU) to try to prevent the body from scarring down the stent. This increases the chances that the Xen® will remain patent and flowing, resulting in lower intraocular pressure.
The Xen® is done in an ambulatory surgery center under light intravenous sedation (like cataract surgery) and usually a local eye block. Following this procedure you will be using post operative medications but initially will be off of your glaucoma drops. Your surgeon will examine you the following day. Like traditional filtering surgeries, your doctor will monitor you carefully the first 4-6 weeks as your pressure can be variable in the early postoperative course. There is no contraindication for patients to undergo MRI with this device following their surgery.
Trabeculectomy

When eye drops, pills, laser surgery, or other less invasive glaucoma surgeries (MIGS) fail to adequately control your eye pressure, your doctor may recommend a more aggressive filtration surgery called a trabeculectomy. This operation works by bypassing the traditional outflow pathway or drain and creating a new drainage pathway using the natural tissues of the eye.
During the operation, the superficial tissue of the eye (conjunctiva) is opened, a flap is created in the underlying thicker tissue (sclera), and a pathway or tunnel is created into the eye by removing a portion of the trabecular meshwork (drain of the eye). The flap is then sutured down to titrate the amount of outflow and the conjunctiva is then closed. This allows fluid in the eye to more readily drain through the created outflow pathway, under the flap, and into a reservoir underneath the conjunctiva (filtering bleb). It is then reabsorbed back into the body, ultimately resulting in lower eye pressure.
The human body reacts to eye surgery as an injury, so its tendency is to scar down or wall of this newly created outflow channel. The surgeon will use anti-scar medication during the procedure, usually mitomycin-C (MMC) or occasionally 5-fluorouracil (5-FU). You will also use steroid eye drops following the surgery to help maintain the patency of the trabeculectomy.
The trabeculectomy is done in an ambulatory surgery center under light intravenous sedation (like cataract surgery) and usually a local eye block. Following this procedure, your eye is generally covered with a patch and removed the next day at your appointment. You will then be using post-operative medications but initially will be off of your glaucoma drops. Following the initial appointment the day after your surgery, your surgeon will examine you weekly for the first couple of weeks. It is important to monitor these surgeries carefully in the initial postoperative period as adjustments can be made for pressures that are too low or too high. If the pressure is too high, it is usually because there is not enough fluid outflow through the tunnel underneath the scleral flap. This flap or valve can be loosened by cutting a stitch in the office using a painless laser, allowing increased fluid outflow, and lowering your eye pressure.
Glaucoma Drainage Implant Surgery
When eye drops, pills, laser surgery, or other less invasive glaucoma surgeries (MIGS) fail to adequately control your eye pressure, your doctor may recommend a more aggressive filtration surgery called a glaucoma drainage implant or tube. It is often performed subsequently to a previously failed filtration surgery such as a trabeculectomy or Xen®. In addition, it might be the best option in particular types of glaucoma such as neovascular or uveitic, as well as eyes that have significant scarring from previous surgeries or injury. Tubes tend to be more resistant to scar formation than other filtration surgeries making them a good choice in these scenarios.
A glaucoma drainage implant or tube is a small prosthetic device that is implanted in the eye, bypassing the trabecular meshwork (traditional outflow drain), allowing fluid to drain from the eye resulting in a lower intraocular pressure. There are a few different drainage implant options and can be grouped into valved (Ahmed) and nonvalved implants (Baerveldt and ClearPath). The valved implants start working immediately when placed in the eye and the non-valved implants are generally tied off or obstructed with a suture, restricting flow initially and allowing the eye to heal prior to the tube opening. Once the suture dissolves or is removed/cut, the tube will begin to drain. Which implant is best for you is a complex decision and is based on multiple factors including the patient, type of glaucoma, and surgeon preference.
Regardless of the implant type, a silicone tube is inserted into the eye, generally in the anterior chamber (space between the iris and cornea). Other locations can also be used. The tube is connected to a plate and acts as a drain, allowing fluid to exit the eye. The plate is anchored to the eye underneath the conjunctiva. The fluid drains into a space between the plate and the conjunctiva and like a trabeculectomy can be referred to as a bleb. It is then reabsorbed into the body resulting in a lower eye pressure. The tube is usually underneath the eyelid and unless the lid is pulled back it should not be noticeable to the patient or their family. You may also notice a small clear or white patch when the eyelid is pulled back. This is a patch the surgeon places over the tube to limit irritation and limit the risk of long term tube exposure through the tissue.
A glaucoma drainage implant is done in an ambulatory surgery center under light intravenous sedation (like cataract surgery) and usually a local eye block. Following this procedure your eye is generally covered with a patch and removed the next day at your appointment. You will then be using post-operative medications and may be using some of your glaucoma drops depending on the implant type and your eye pressure at that visit. Following the initial appointment the day after your surgery, your surgeon will examine you closely for the first few weeks adjusting your eye drops as needed, particularly with the non-valved implants prior to them opening as discussed above.

