Optic Nerve Exam
Using our microscopes and high power lenses, as well as an instrument called an ophthalmoscope, the optic nerve is readily examined in the clinic setting. The nerve consists of over a million nerve fibers which originate in the retina and transmit information to the brain to allow us to view the external world. The optic nerve is shaped like a doughnut, with the rim being composed of these fibers and a central empty space or optic cup. In glaucoma we see atrophy or loss of these nerve fibers, resulting in loss of the rim and enlargement of the cup (hole of the doughnut enlarges). In glaucoma, the optic nerve generally has thinner rim and larger cup, whereas a normal optic nerve has a thicker rim and smaller cup. The optic nerve exam alone is crucial to help diagnose glaucoma as well as assess if the disease is stable or progressing.
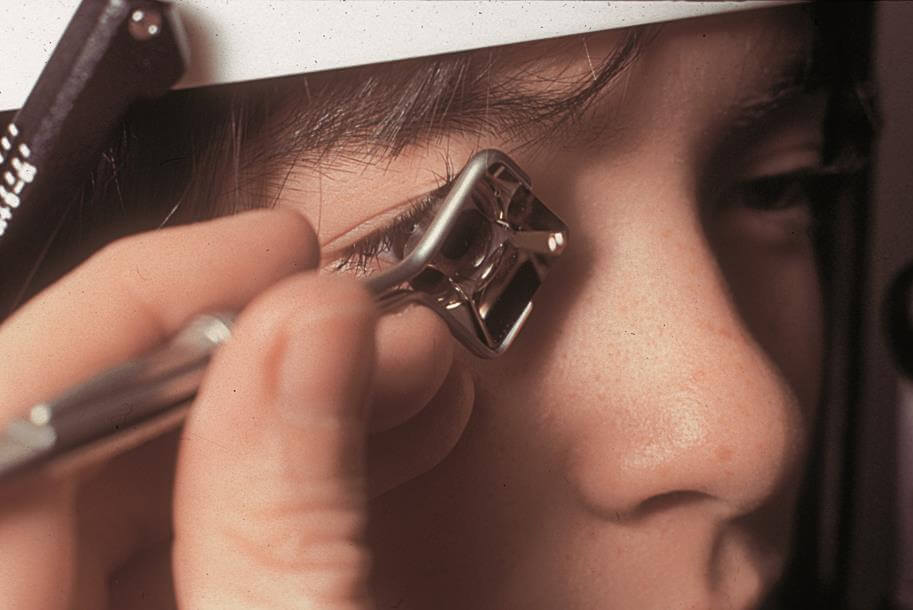
Gonioscopy
The eye is a pressurized system, with fluid being pumped into the eye and subsequently being drained inside the eye. This system of drains begins in the front part of the eye, an area called the anterior chamber angle (space between the iris and cornea). The structure in the angle called the trabecular meshwork is the opening of the drain. Gonioscopy assesses the angle to see if it is open for the fluid to reach as well as make sure there are no abnormalities (scarring, abnormal blood vessels etc). When the angle is narrow or closed, the risk of glaucoma is increased. To do this, the doctor will use an instrument called a gonioscopy lens, which allows visualization of the anterior chamber angle at the microscope.
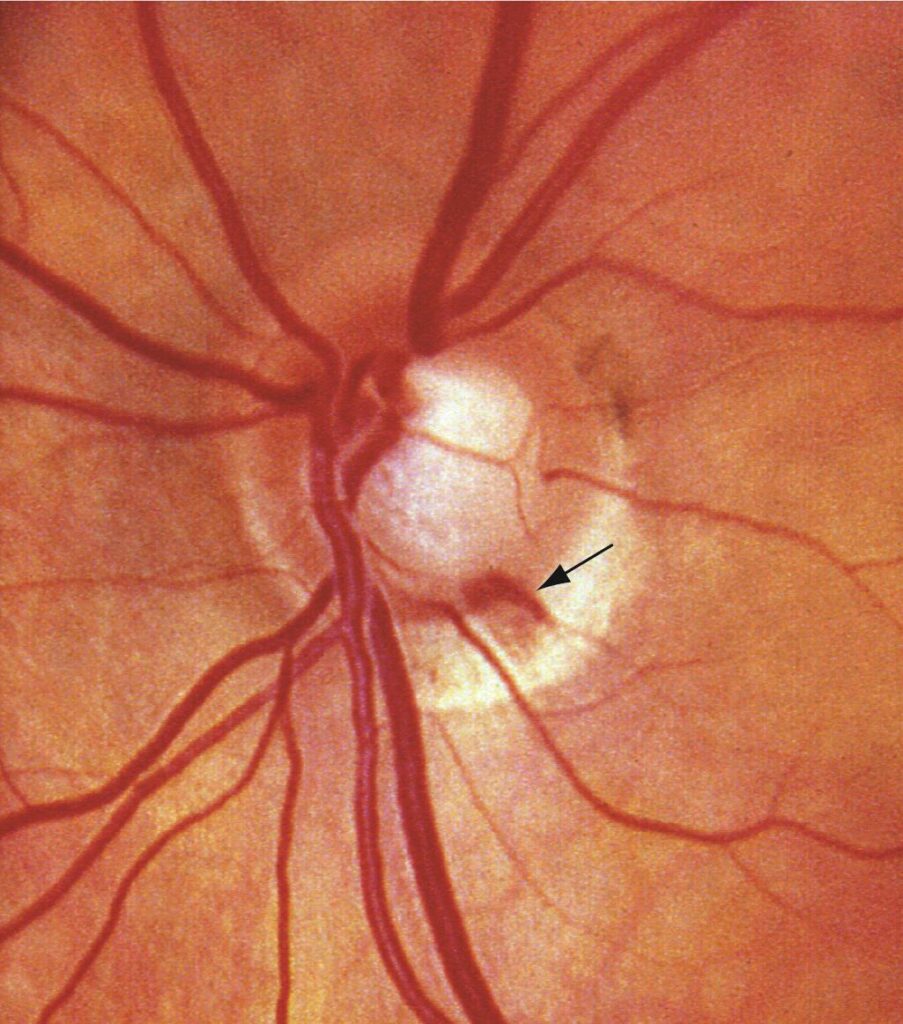
Fundus Photography
Using a special type of camera, a high power magnified photo of the optic nerve can be obtained. This helps aid in the diagnosis of glaucoma, but can also be used to assess for changes in the optic nerve (glaucoma progression) over time and is very useful to pick up optic nerve hemorrhages (another sign of possible progression). It is a simple yet crucial tool in glaucoma diagnosis and management.
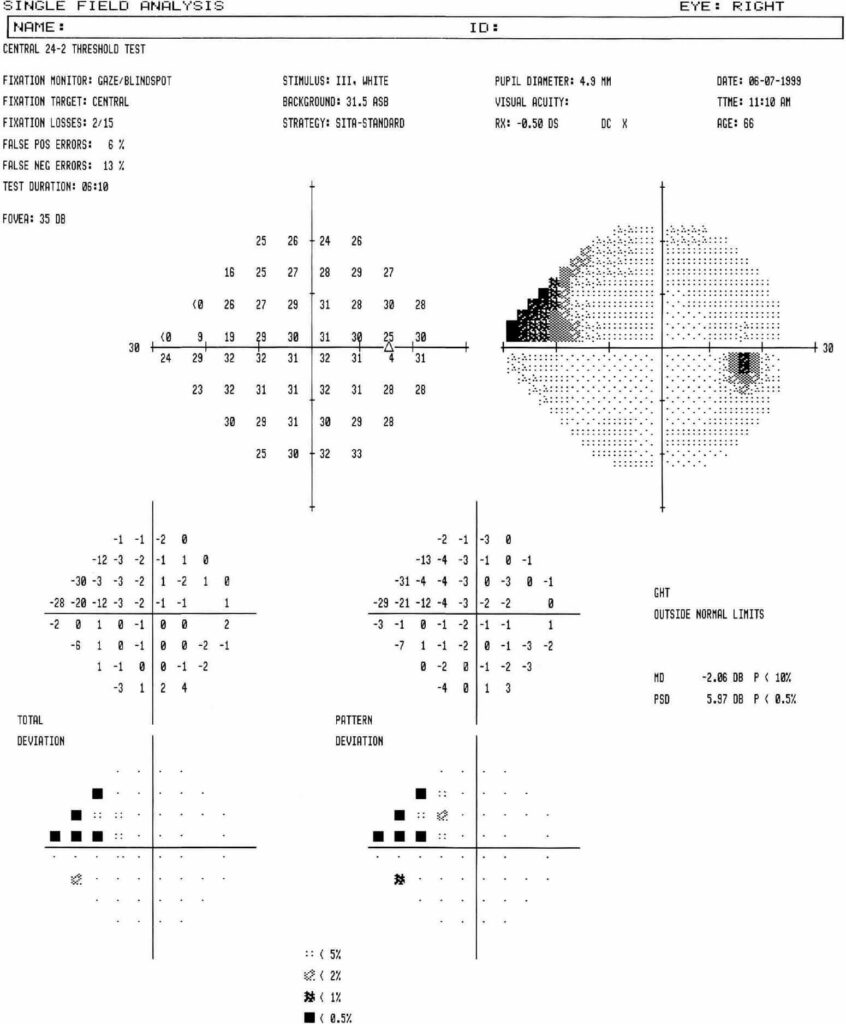
Visual Field Testing

Visual field testing is a very important tool to both diagnose as well as assess for glaucoma stability or progression over time. Glaucoma causes loss of our visual field, often peripheral vision first and eventually our central vision if not adequately treated, resulting in blindness. It can also cause loss of more central vision early on. The device will test a series of lights throughout one’s visual field providing a very important measure of the degree glaucoma severity. The test will be administered by one of our technicians and the results will be reviewed with you by the doctor. Although the test can be challenging, long, and occasionally frustrating, it is crucial in glaucoma diagnosis and management.
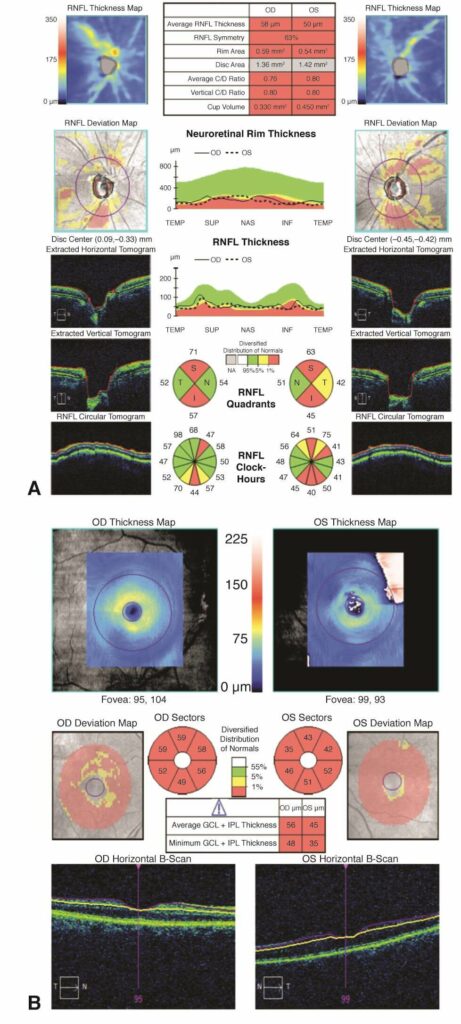
Optic Nerve Fiber Analysis
Optical Coherence Tomography (OCT) is a device that gives us a quantifiable measurement of the nerve fiber layer, which is damaged in glaucoma. This technology has enabled us to measure on the level of microns the nerve fiber layer and can identify areas of thinning or damage to the optic nerve. In addition to helping diagnose glaucoma, it can be used to assess disease progression over time, which would manifest as loss or thinning or the nerve fiber layer. The test is administered very quickly by our technicians, and only requires the patient to fixate on a light. OCT can also be used to assess retinal problems such as diabetic eye disease and swelling in the retina due to a stroke in the eye.